This chapter focuses on volumetric (3D) imaging; multi-detector and cone beam computed tomography (MDCT and CBCT respectively).
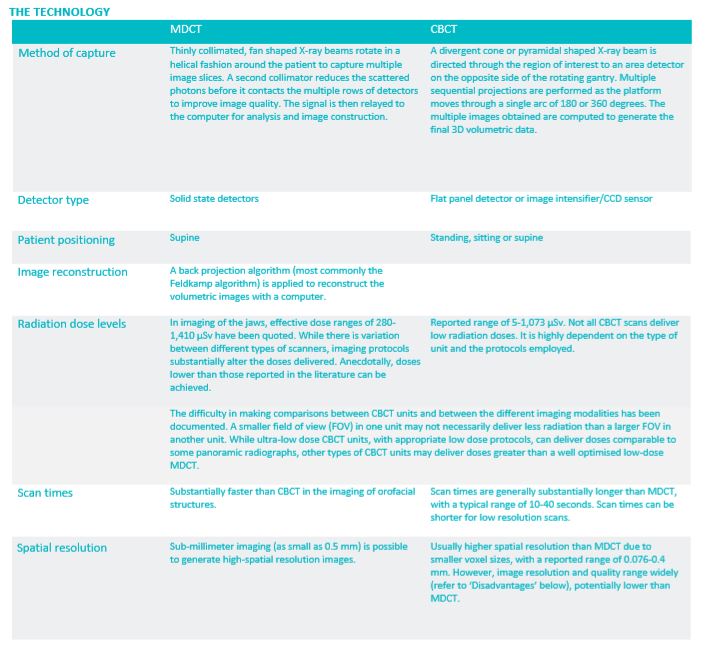
The following table compares MDCT and CBCT technology.
TECHNICAL ASPECTS
MDCT machine operation should only be undertaken by an appropriately trained radiographer/radiologist.
The technical aspects of CBCT has been covered in various texts. Adequate training is essential, including a thorough understanding on the influence of protocols on image quality and radiation safety. The basic principles of reducing radiation exposure were discussed in Chapter 1. The following highlight some of the key issues in relation to CBCT:
• Field of view: –
Selecting the smallest FOV for the region of interest (ROI) will improve the image quality and potentially significantly reduce radiation dose.
– Large volume CBCT generally produce moderate resolution scans which may not be sufficient for fine detailed tasks such as examining nondisplaced tooth fractures or small root canals. High resolution small FOV CBCT may be more appropriate in such cases. Higher resolution scans are generally associated with higher radiation doses. – The FOV is limited by the size of the detector. Some units are capable of scanning a ROI which is larger than the FOV of the machine by stitching multiple scans together. However, this will result in an increased radiation dose and acquisition time. One scan with an appropriate larger FOV machine is therefore generally recommended over stitching of multiple scans.
• Voxel size: Smaller voxel sizes capture less X-ray photons, which results in images with more noise. Most CBCT units compensate for this by increasing the radiation dose.
• Frame rate: The more basis projection images captured, the more data available for reconstruction. This improves spatial and contrast resolution, decreases noise and reduces metallic artefacts. However, it increases patient dose, and also increases scan times with associated potential for motion artefact.
• Trajectory arc: Reduction in the rotation arc from 360 to 180 degrees will reduce the radiation dose by 50%. However, this will have a corresponding decrease in image quality.
• X-ray generation: Using a pulsed X-ray beam to coincide with detector sampling will reduce patient exposure by up to 50%
ADVANTAGES
3D volumetric imaging overcomes the limitations of 2D imaging (superimposition, geometric distortion and magnification). The data from a single scan can be reformatted to be viewed along the axial, coronal, sagittal or any other plane (multiplanar reformatted images). Surface rendering facilitates viewing of the data as 3D virtual ‘models’.
Compared with 2D plain films, CBCT and MDCT have both been found to be more accurate in measurements in any dimension. Several studies have found CBCT and MDCT linear measurements (over lengths comparable to a tooth) to be accurate within 1mm.
CBCT potential advantages:
• Easier accessibility, usually lower cost and smaller physical footprint than MDCT.
• Potentially lower radiation dose than MDCT. It must be noted CBCT scans can deliver relatively large radiation dose levels, potentially higher than a low dose MDCT scan (refer to ‘The technology’ on page 13).
• High osseous/calcified structure spatial resolution due to smaller voxel size, which can better depict bony trabeculae, root structure etc.
MDCT potential advantages:
• A more powerful and flexible imaging modality. • Visualisation of soft tissues and scans with or without intravenous contrast may be critical in some cases.
• High contrast resolution, such that tissues with even 1% difference in physical density can be identified. • Improved image quality due to better signal-to-noise ratio.
DISADVANTAGES
CBCT is subject to more detrimental effects on image quality than MDCT:
• Increased noise compared to MDCT: – A result of Compton scattering. The amount of scattered radiation is proportional to the volume of tissues in the X-ray beam, and can be reduced by decreasing the FOV.
• Poor soft tissue contrast: – The contrast resolution is limited to bony or calcified structures. CBCT has less overall contrast resolution than MDCT.
• Beam hardening: – Preferential absorption of lower energy photons through dense objects results in distortion of objects, appearance of bands or streaks (extinction or missing value artefacts) which can contribute to misinterpretation of the scan. The size of the patient’s head as well as the density of the object also contribute to the degree of beam hardening
• Motion artefacts: – Occurs if the patient is unable to keep still for the entire scan time. This is a common problem as CBCT scan times are generally substantially longer than with MDCT. Selection of a shorter scan time may reduce this, but a decrease in scan time reduces image quality.
• Metal streaking artefacts: – The absorption of nearly the entire X-ray beam energy by metallic structures results in an opaque streak. This may obscure key structures.
• Cone-beam effect: – The peripheries of the image are subject to more image distortion, streaking artefacts and greater noise.
• Moire artefact: – Too few basis projection images occur resulting in undersampling of the object.
• Scanner related artefacts: – Appears as a circular streak, often due to poor calibration or imperfections in scanner detection.
• Inaccurate bone density estimation: – The grey values in CBCT cannot be quantified as Hounsfield units (HU), which measure the relative density of body tissues based on a calibrated greylevel scale. This is possible with MDCT.
The main limitations of MDCT are the potential for higher radiation doses, and reduced accessibility. In some cases, the MDCT image quality of teeth and osseous structures is comparable or better than CBCT scans. However, high resolution small FOV CBCT scans for persons who are not particularly large (with no motion artefact) produce higher quality images of the jaws and teeth than MDCT scans.
APPLICATION
In general, the prescription of 3D imaging should only be carried out in cases where lower dose imaging techniques are not able to provide the information required for diagnosis and treatment planning. Without specific indications, 3D imaging for routine screening is not recommended.
In recent years, there has been an increase in the use of CBCT in dentistry, primarily related to improved understanding of the application, accessibility and dose considerations. While a few authors consider that it has largely replaced MDCT for dentistry, the limitations of CBCT require consideration and it is not the optimal modality for many cases. Understanding of the strengths and limitations of both CBCT and MDCT is necessary for selection of the most appropriate radiologic test. In some instances, other modalities such as MRI, ultrasound or nuclear medicine may be optimal. The indications for a CBCT/MDCT image has been outlined by various bodies. These position statements and guidelines will alter as the research in this field continues. The prescription of volumetric imaging, in relation to intraoral radiography (IOR) and OPG has been discussed in preceding chapters. The following discusses the more common application of CBCT and MDCT in dentistry:
• Despite its increased sensitivity for the detection of dental caries, CBCT has low specificity and is associated with a higher radiation dose than bitewing radiography. As such, it is not recommended as the primary imaging technique for dental caries. Also, metallic artefacts and beam hardening from adjacent restorations render CBCT inadequate for caries detection.
• MDCT and CBCT are more accurate than IORs and OPGs at identifying the severity of periodontal bone loss and infrabony defects, detecting furcation involvements and providing information on root morphology. With the associated contribution to diagnosis and prognosis, it has been suggested that treatment time and cost may be reduced with the better ability to make appropriate treatment decisions on whether to extract or maintain periodontally compromised teeth. However, it remains important that 3D imaging for periodontal disease should only be applied when clinically indicated.
• CBCT and MDCT have been shown to be more sensitive in the detection of periapical lesions. However, IOR may suffice in many cases. Several authors consider that limited FOV, high resolution CBCT should only be considered in cases where there are contradictory clinical and radiographic signs and symptoms, nonspecific or persistent pain, complex root morphology or extra canals, surgical planning and suspected vertical root fracture not detectable with 2D radiography. The application of MDCT and MRI must also be considered.
• Potentially more complicated or difficult extraction cases may require volumetric imaging, particularly when plain film suggests the tooth is in close proximity to critical structures, such as the mandibular canal or maxillary sinus. While the presence of any of Rood and Shehab’s1 criteria may warrant further radiologic examination, it has been shown that the absence of these radiologic signs does not preclude a close relationship with the inferior alveolar nerve. Diagnostic imaging, including 3D imaging, should only be performed where it has the potential to contribute to diagnosis, prognosis, treatment planning or influences a planned procedure.
• Most authors consider that volumetric imaging should be used in implant planning. Where required, virtual planning and fabrication of computergenerated surgical guides can be performed, based on the scan data sets.
• When indicated, volumetric imaging has been recommended for the assessment of sinus anatomy or pathology, and the preoperative assessment for sinus augmentation or grafting procedures. Plain film imaging for paranasal sinus disease is insufficient. Presently, MDCT remains the most commonly used modality for paranasal sinus disease, considered to be the optimal technique by most clinicians and surgeons.
• MDCT and MRI are appropriate for the evaluation of the bony and soft tissue structures of the TMJ respectively. Some consider that CBCT may be more suitable if soft tissue imaging is not required due to its high bony spatial resolution and reported lower radiation, but factors affecting the image quality must be considered (refer to the aforementioned ‘Disadvantages’), especially beam hardening and the relatively low signal-to-noise ratio associated with CBCT scans. Inappropriate selection of the imaging modality can lead to misdiagnosis and a delay in appropriate management.
• MDCT has been recommended over CBCT for more complex, serious or significant cases, especially where there is potential soft tissue involvement. The list includes benign or malignant tumours, cysts, undiagnosed pain, facial fractures, cellulitis, osteomyelitis or osteonecrosis of the jaw. Other tests, including MRI, ultrasound and nuclear medicine must also be considered.
• CBCT use in orthodontics for diagnosis and treatment planning is becoming increasingly popular, but due consideration should be given to the increased lifetime risk of radiation exposure in children/adolescents. Not all CBCT scans are low dose (refer to ‘The Technology’ on page 13). The appropriate low dose CBCT unit together with appropriate protocols must be employed. Common applications include assessment of impacted canines, root resorption, tooth position and morphology, and craniofacial anomalies.
• It has been reported that volumetric imaging is more accurate than 2D plain radiographs in the evaluation for obstruction in the upper airways and craniofacial structures. Radiological tests, including 3D imaging, should be prescribed only where it has the potential to contribute to diagnosis, prognosis, treatment planning or influences a planned procedure
INTERPRETATION
• The interpretation of CBCT or MDCT scans require a higher level of knowledge and skill sets than plain film. Prerequisite knowledge includes radiologic anatomy, orofacial pathology, radiologic features of pathoses and a thorough understanding of the limitations of the technique. Appropriate image interrogation is critical. Some authors recommend that these scans should be interpreted by persons with sufficient advanced training. Interpretation is discussed in Chapter 5.
Published on March 15, 2021
Back