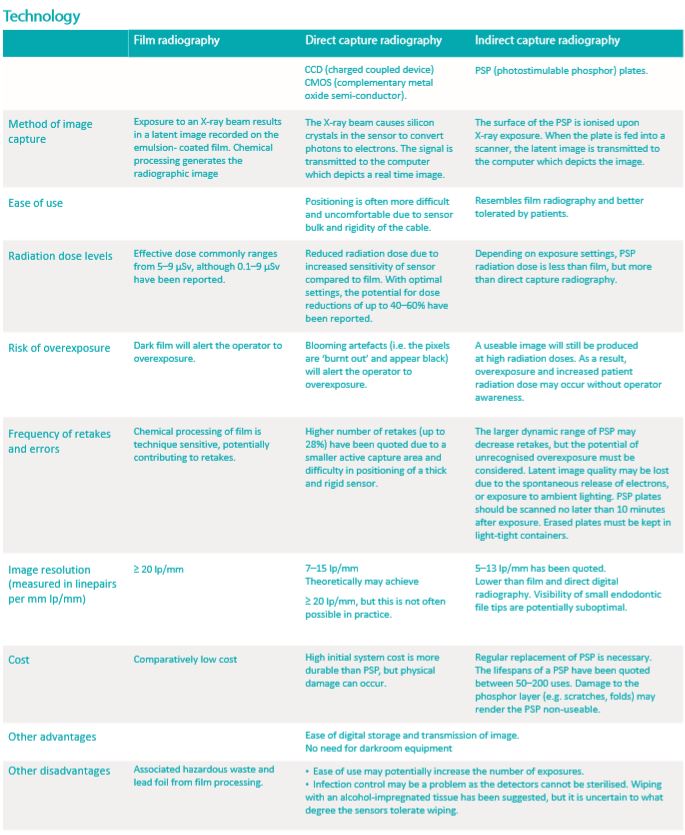
This chapter focuses on intraoral 2D radiography, namely periapical and bitewing radiographs. The table below compares intraoral radiography technology based upon the type of detector.
REDUCING RADIATION EXPOSURE
The following summarises some of the ways in which dose minimisation can be achieved: • Adopt the principle of ALARA (as low as reasonably achievable).
• Review relevant previous studies prior to further imaging. Request from previous clinician if necessary. • Use the fastest image receptor compatible with the diagnostic task (F-speed film or digital).
• Benefits associated with the use of lead aprons have been shown to be minimal compared to other methods of dose reduction. As such, this could be considered optional unless required by relevant governing bodies.
• Thyroid shields have been shown to reduce thyroid radiation dose.
• Rectangular collimation has been suggested, substantially reducing dose. However, it is technically more demanding, and its use must be balanced against the possibility of repeats, potentially increasing the overall dose delivered.
• Use a film positioning device to aid in the parallel alignment of the film with the collimated beam to minimise geometric distortion and for reproducibility of subsequent radiographs. • Use optimal settings to minimise exposure times.
• Minimise the number of images necessary to obtain essential diagnostic information. • Optimal film exposure and processing technique.
• Implement quality assurance protocols to regularly evaluate the film processor, image receptor devices and processing chemistry.
The justification and selection criteria for intraoral radiographic examination have been thoroughly outlined by various bodies, including the American Dental Association and the European Commission. A radiologic examination should be undertaken only when it provides additional information about a condition or planned procedure and/ or influences management or surgical approach. Other factors, including the patient’s history and susceptibility to dental diseases should also be considered. The benefit must outweigh the accumulated biological risk to the patient.
The clinician needs to prescribe the optimal technique based on clinical indications. The practise of initially prescribing conventional examinations (e.g. plain film 2D radiographs) before determining whether 3D volumetric information is needed has been suggested. However, the limitations of 2D imaging (geometric distortion and projection errors, overlapping of anatomical structures and image magnification) have been well documented and may lead to difficulty with diagnosis and misinterpretation of results. In situations where 2D radiography is neither sufficiently sensitive nor specific, or multiple exposures are required to visualise an area, more advanced techniques should be considered
In the following subsections, brief references to cone-beam computed tomography (CBCT) and multi detector computed tomography (MDCT) are made where relevant. Chapter 3 addresses volumetric techniques in more detail.
APPLICATION
Bitewing radiographs The bitewing (BW) radiograph remains the most optimal technique for detecting interproximal caries but may not be necessary in patients who show no evidence of the disease, have open proximal contacts or a low caries risk. Diagnosis should be made in conjunction with a clinical examination as low sensitivity (0.24–0.42) and high specificity (0.70–0.97) have been reported. The frequency of their prescription should be determined based on caries risk assessment and altered as the individual circumstances of the patient changes with time.
Several studies have reported that CBCT may be useful for caries detection but is not recommended as the primary technique for caries diagnosis on account of the potential for higher radiation dose, low specificity and beam hardening artefacts when metallic or radiodense restorations are present.
Furcation defects and the more superficial periodontal bone can be demonstrated in a BW, which is taken at right angles to the X-ray beam.
Periapical radiographs For periodontal disease, the periapical (PA) radiograph demonstrates a 2D view of periodontal bone and root morphology, with associated limitations. Foreshortening or elongation of the teeth occur, resulting in distortion and inaccurate assessment of the true horizontal bone height.
Image distortion is worse when using a bisecting angle technique. Limited sensitivity for measuring the degree of periodontal bone loss, mapping infrabony and vertical defects and the assessment of furcation involvements have been reported. The existence and severity of bone loss demonstrated in one imaging episode does not indicate active disease. Therefore, radiological examinations should be correlated with clinical findings, and compared with previous imaging where relevant. Increasingly, for more complex cases, the use of volumetric (3D) imaging has been suggested to allow for more accurate detection, diagnosis, prognosis prediction and treatment planning.
For periapical disease, a PA radiograph correlated with clinical findings is generally sufficient for most cases. However, the limitations of these 2D views must be recognised. It has been shown that MDCT and CBCT are more sensitive for the detection of periapical lesions.
For the initial diagnostic stages of implant planning, PA radiographs may be helpful as a preliminary guide on bone availability and proximity to anatomical structures. However, PA radiographs are insufficiently accurate for the final planning for implant placement. The 3D morphology and relationship to relevant structures is not demonstrated. In this regard, volumetric imaging techniques are superior and generally accepted as the modalities of choice.
PA radiographs have been recommended for the measurement of baseline bone levels after implant placement. It is obvious that 2D radiographs only demonstrate the proximal periimplant bone and optimal paralleling technique is essential. CBCT and MDCT may be useful in some cases, but are not without their limitations, namely the adjacent artefact.
For most cases of dental trauma, at least two PA radiographs with different horizontal and vertical angulations have been recommended. They may be sufficiently accurate for minor dental injuries, but low sensitivity in detecting fractures have been reported. CBCT and MDCT may not be essential for acute management of minor dento-alveolar trauma. These techniques, usually low-dose protocol CBCT, should be considered where 2D radiography is inconclusive. Volumetric imaging could also be considered in the long-term management of trauma cases.
Other situations requiring volumetric imaging include cases with unresolved symptoms and more serious trauma, especially where injuries extend beyond the dento-alveolar complex. MDCT is the modality of choice over CBCT for more complex cases.
The information provided by a PA radiograph may be insufficient for surgical and/or orthodontic treatment planning for impacted canines and their relationship to adjacent structures. Ultra-low dose CBCT is emerging as a modality of choice, as it is able to demonstrate the precise location and morphology of the tooth, the surrounding structures and detection of root resorption of adjacent teeth.
Overall, there are increasingly fewer indications for vertex occlusal views as well as the full mouth series with the advent of CBCT. Volumetric imaging is discussed in Chapter 3.
VIEWING CONDITIONS
To ensure the highest diagnostic accuracy, it is important to review radiographs under optimal conditions. Low ambient lighting (no more than 50 lux), a bright backlight source and magnification is recommended for film radiographs. Use of a mask to reduce glare from light boxes around the film is also helpful. With more steps involved in digital image acquisition and display, any component in this process can influence the quality of the final image.
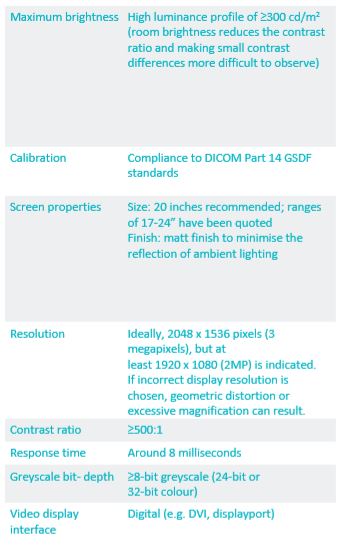
Display monitor:
With advances in commercial display monitor technology, these monitors (with correct specifications – see below) are comparable with medical grade monitors for most diagnostic purposes.
Graphics card:
• Should be appropriately matched and of high quality to avoid information loss and inferior quality images.
Image enhancements and manipulation:
• Zoom control may aid in radiologic diagnosis of proximal carious lesions. It has been suggested that the optimum magnification should be no more than six times the original.
• Enhancement of density and contrast may improve diagnostic accuracy.
• Inverting greyscale values has not been found to improve diagnostic accuracy. Instead, it may hinder dentinal lesion detectability.
• Pseudo-colour enhancement has not been documented to aid diagnosis
Storage and transmission:
• The image should be stored in its original, uncompressed format with an automatic backup function. Minimising compression of the radiographic image during transmission is necessary to avoid loss of relevant data.
Printed copies of radiographs compromise diagnostic accuracy and are not recommended. They are highly dependent on the quality of printer and paper and will not demonstrate the same optical range as film or high-quality monitors.
INTERPRETATION
The importance of applying a methodical approach to radiological interpretation is critical.
Published on March 12, 2021
Back